 How does thermal imaging work?
How does thermal imaging work?
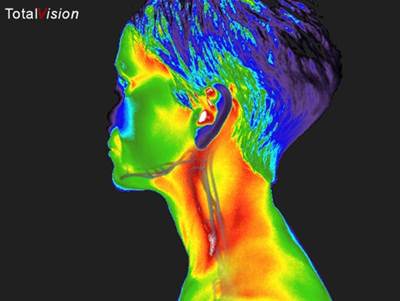
Thermal imaging is a 15 minute, non-invasive test of physiology. Thermal imaging uses a highly sensitive, high-resolution digital thermal camera to take a picture of your body’s infrared heat and display these patterns in the form of a digital image. The cells of your body produce heat through their normal function. Abnormal cells typically produce more heat in the early stages of development (before a tumor forms).
Before most tumors grow, abnormal cells will:
• stimulate new blood vessels to grow
• re-open unused blood vessels
• maintain those blood vessels already in use
The cells build a vast network of blood vessels in the area it will ultimately grow. A tumor needs more blood flow than normal cells to support its rapid growth. With more blood flow, there is more heat. Thermal imaging examines these “hot spots” which can be the early warning signs of developing pathology. This activity has been shown to begin years before a tumor forms, and before any warning signs can be given by other screening methods.
Thermography is a totally non-invasive procedure that is completely safe. There is absolutely NO contact with the body, NO compression, and NO radiation. While a variety of studies have called into question the safety of cumulative exposures to radiation, this is not the case with thermography. Thermography emits nothing. It is simply a picture of your unique thermal heat patterns.
Who can benefit from breast thermography?
Breast thermography is a great option for all women but particularly women that fall into certain categories. Women with dense breast tissue, fibrocystic breasts, as well as women with implants or women that have had mastectomies without reconstructive surgery are more difficult to screen for breast cancer using other screening technologies. However, that is not the case with thermography. Since the screening process is nothing more than taking pictures or images of the infrared heat emitted from the body, the size of the woman, size of the breasts or tissue type are no longer concerns for the sake of breast screening. This test can provide a clinical marker to the doctor or practitioner in the event that a specific area of the breast needs particularly close or frequent examination.
Who reads the images and writes the reports?
Our images are sent to a professional group of physicians who are trained in the protocols of reading thermal images. A formal interpretation and written report, including color images, is prepared and sent to you in approximately two weeks. If quicker results are desired, rush service is available for a fee. We are happy to send a copy of your report to your doctor upon request.
What does the procedure involve?
This quick and easy procedure starts with you undressing from the waist up and changing into a hospital gown to allow air to circulate which allows your body temperature to cool down. Cooling time is approximately 12 minutes. While you are cooling, you will be asked to complete several forms including a brief medical history. Once acclimated, you will be asked to sit in front of the camera, with your hands behind your head. Five different images will be taken. This allows the camera to scan the breasts, neck and underarms as well as the lymph nodes under the arms, breasts, and neck. These images are then sent for interpretation and archived for future comparison. The average visit is 30 minutes.
Why do I need to establish a baseline?
After your initial set of breast scans, it is highly recommended that you return for a second set of scans three months later. This second set of images will be compared to the first set of scans, and assures that your thermal patterns have remained unchanged. It is important to determine an accurate picture of your unique thermal heat patterns so that even the most subtle changes can be identified as soon as possible.
What is the difference between thermography and mammography?
Thermography detects the subtle physiologic changes that accompany breast pathology, whether it is cancer, fibrocystic disease, an infection, or vascular disease. It can alert you and your doctor to changes that can indicate early stage breast disease. It is safe, effective, and ideal for women of all ages. It is completely non-invasive and does NOT use radiation. It is a “do no harm” approach to routine breast screening.
Mammography is a test of anatomy that uses x-ray to look for masses or lumps. These masses can take years to form – sometimes 5-10 years before they are large enough and dense enough to show up on an x-ray. Although touted to be harmless, mammograms do involve compression of the breast tissue, which may be uncomfortable for some women. A dose of radiation is administered with each view taken.
Will I still need to have a mammogram?
While thermography is a great basic screening method, it looks at the breast tissue differently than a mammogram does. For some, thermography is an adjunctive procedure and is used in conjunction with the annual mammogram and/or ultrasound. For others who may not be candidates for mammography or choose not to use mammography, thermography is a great option. Mammography can be a very useful follow up tool when warranted. When used in conjunction with thermography, the rate of early detection is increased to as much as 95%.
In the event that something suspicious should appear on your thermogram, your doctor or health care practitioner should be consulted immediately. After a thorough discussion of your options, you and your doctor or health care practitioner may decide that a mammogram or ultrasound is warranted for a different view of the area of concern.
Can thermography diagnose breast cancer?
No. In fact, all other screening methods (mammography, ultrasound, physical/self-exam) can only suggest the presence or absence of disease. The only way to diagnose breast cancer is through a biopsy and pathological study.
How accurate is thermography?
Thermography has a sensitivity and specificity rate of approximately 90%. As with any test, results are often only as good as the technician performing them. Don’t hesitate to ask how much experience your technician has with the equipment and the performance of the procedure. A positive thermogram can be the single most important marker of high risk for developing breast pathology.
Why does my doctor not know about or recommend thermography?
Unfortunately, many doctors either don’t know about this technology or have out of date information as to its efficacy and benefits. If your doctor would like to receive a copy of the most current research data regarding breast thermography, please have them contact our office.
Is this procedure covered by insurance?
This all depends on your individual insurance plan. Some companies cover the procedure while others do not. Our policy is to collect payment at the time of service while providing you with a receipt appropriate for filing with your insurance company for reimbursement. Thermography is not covered by Medicare, Medicaid, or Tricare.
